Introduction: Hematological involvement (HI) is a life-threatening involvement of Langerhans cell histiocytosis (LCH). Since 1975, its definition is based on the Lahey criteria: Anemia (Hb <10 g/dL and <9 g/dL in infants) and/or thrombocytopenia (platelet count <100x10 9/l).
Methods: Among 2,234 patients < 18 years enrolled in the French histiocytosis registry (cutoff date May 2023), 303 patients presented HI. We differentiated mild HI (MHI) (Hb > 7 g/dl and Platelets > 20x10 9/l) from severe HI (SHI) (Hb ≤ 7 g/dl and Platelets ≤ 20x10 9/l) by using usual cutoffs for transfusion requirements.
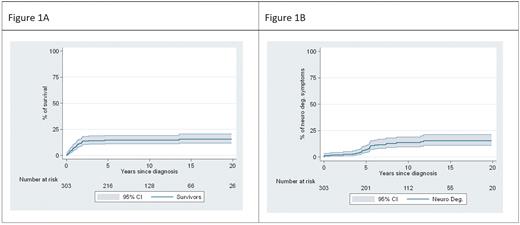
Results: Median age at diagnosis was one year and sex was male in 49%. The median follow-up in the 258 survivors was 10.9 years, while death occurred after a median of 0.9 years in the 45 patients who died (Figure 1A). Only 3 patients died later than two years of initial diagnosis. The HI was mild in 150 cases and severe in 153 cases. BRAF v600E was found in 88 among the 101 patients for which mutation analysis was documented. Patients with SHI had significantly more lung involvement (35 % vs 19 %), more hepatic involvement (72 % vs 21 %), and more skin involvement (85 % vs 61 %). Morphological bone marrow infiltration by CD1a positive cells could not differentiate between SHI and MHI and bone marrow features were hardly informative. Signs of myelofibrosis were documented in 9 patients mostly later in the disease course. Lastly, 44 macrophage activation syndromes were observed exclusively in SHI. For 11 of those patients panel analyses of hemophagocytic lymphohistiocytosis genes did not show any bi-allelic pathogenic variants. 20 patients did not receive any therapy, including one with SHI and 19 with MHI. An intensive approach with hematologic stem cell transplantation (HSCT) (n=11) and 2-Cda-Cytarabine (2-Cda-AraC) (n=44) was proposed almost only for SHI. MAPK-inhibition was used in 40 patients. Three deaths were observed among the MHI and 42 among the SHI. From 1983 to 1998 mortality was about 50% and 30 of 63 patients died. With the establishment of the second-line treatment by 2-Cda-AraC mortality decreased drastically and from 1998 to 2014 only 13 of 194 patients died. From 2014 on patients received exclusively MAPK-inhibition as second line treatment and 2 of 46 patients died (one without therapy, one at the initiation). The overall survival is depicted in figure 1A. Neurodegenerative (ND) complications were observed in 32 patients (10.5%) with a median delay of 4.8 years after initial LCH diagnosis and incidence of ND was independent of the MHI or SHI group (Figure 1B).
Conclusion: In Langerhans cell histiocytosis, the classic definition of hematological involvement by the Lahey criteria should be reconsidered. HI may be limited to severe HI that included almost all medical complications and warrants innovative approaches, while mild HI can be managed by the classic therapeutical approach. Even if progress has been achieved in the treatment of LCH patients with HI with more than 95% achieving short-term control, long term neurodegeneration remains a challenge in this group of patients, which warrants further research.
Figure 1: A) Kaplan-Meier curve of cumulative incidence of death for all the 303 patients, regardless of therapy. B) Risk of clinical neurodegenerative symptoms in the same cohort (considering death as a censor).
OffLabel Disclosure:
No relevant conflicts of interest to declare.
Braf inhibitors and other MAPKinase inhibitors inrefractory langerhanscell cell histiocytosis

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal